I have meant to blog about this for a while, but it always takes a couple of really whopper cases of something to move me in that direction, and last week was no exception. I saw probably one of the worst case of post breast surgery pain that I have seen in a decade.
When I graduated from school 29 years ago. It never occurred to me I would be working on feet and breasts as much as I do. When you consider that 20% of the American adult population suffers from daily impairing foot pain, the foot work should not come to you as a surprise, but the work on the chest wall and breasts associated soft tissues probably will. The reality I encounter in practice is that a lot of women will have breast surgeries for variety of reasons: mostly mastectomies or lumpectomies for breast cancer, breast reconstruction surgeries, and some elective surgeries.
Thankfully, when you consider the sheer number of women having breast surgeries every year, a lot of them will come through the experience with full recoveries and no further issues. However, even with the small percentage of women having complications, that is still an enormous amount of women walking around with daily discomfort in the area of the breast itself, the armpit, the anterior neck and shoulder, and sometimes down the arm.
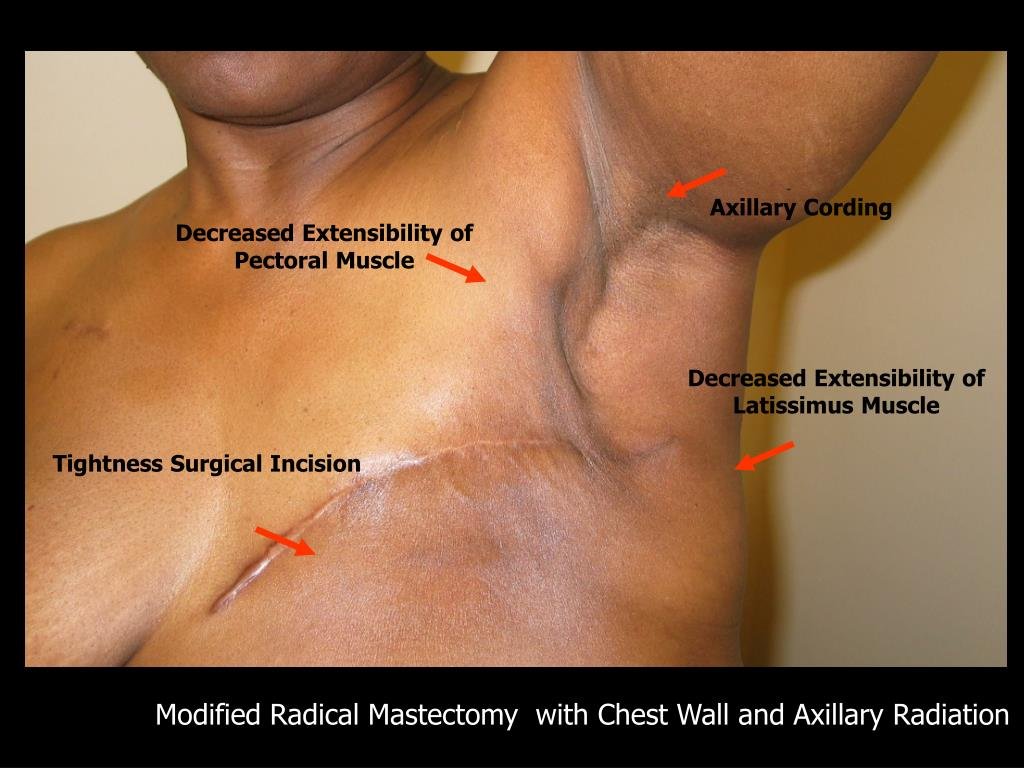
The most common issues I tend to run into and hopefully address in women post breast surgeries are the following:
– Pain along the anterior neck, upper back, and shoulder blade. This is often the result of generalized shortening of the anterior tissues in the chest wall, post surgery scar tissue, and immobilization, causing some anterior jutting and internal rotation of the shoulder, pulling on the shoulder blade.
– Pain along the breast tissue itself, most commonly along the lateral breast, chest wall, and axilla. This is most commonly associated with scar tissue formation on the lateral aspect of the breast. This is often associated with a phenomenon referred to as "chording", which refers to a form of scar tissue formation that looks like the strings of a musical instrument.
– Pain or tingling, numbing down the arm. This is often mistaken for secondary cardiac complication and leading to multiple cardiac testing and chest CAT scans. The scar tissue from the breast surgery and the immobilization can lead to some strangulation of the neurovascular bundle in the axilla. Patients will often have a shooting tingling pain down the triceps, as well as a sensation of hot and cold in the arm that remains unexplained.
– Continued uncomfortable swelling in the armpit to the upper arm, from lymphedema associated with scar tissue obliterating normal lymph return.
The treatment for these issues boils down to several concurrent interventions including:
– Chiropractic adjustments to the neck, thoracic spine, shoulder blade, and shoulder.
– Rehabilitative exercises to restore normal alignment of the shoulder girdle.
– Intense soft tissue scar manual therapy, to improve normal lengthening and flexibility of the affected tissues. This would include specific nerve to soft tissue manual adhesion release therapy, which often produces lasting relief of chronic breast and arm pain.
– When necessary lymph drainage therapy.
– Home self-care including knowing how to stretch, sometimes self treatment of soft tissue adhesions.
– Sometimes supportive home measures such as sports taping of the breast to improve normal realignment of the breast tissue towards midline and avoiding crowding of the armpit where the neurovascular bundle to the arm is located.
– Picking out the right bra going forward to properly support and shift the breast implant material post mastectomy scar.