A special note about osteoporosis and diet, because it is an area of high confusion.
For most folks, the connection between diet and osteoporosis is reduced to getting a defined amount of calcium in your diet or through a supplement. Our bodies do need a minimal amount of absorbable calcium but there is much more to it. And supplements need to be in the right form to be of value (that will be in a later blog.) ALSO, REMEMBER THAT NUTRIENT INTAKE AND BONE AVAILABILITY ARE DEPENDENT UPON PROPER ABSORPTION IN THE GI, WHICH CAN BE IMPAIRED BY A VARIETY OF CHRONIC GI PROBLEMS AND MANY COMMON MEDICATIONS.
CALCIUM: There is individual variation of how much one person needs, but retrospective population studies of folks who have eaten a traditional diet shows they were getting anywhere from 800-1600 mg. Calcium sources are probably the most important factors. Calcium from whole foods that contain some of the other nutrients that are incorporated in bones are the best. For people who have good tolerance to dairy products, cultured dairy (cheese, yogurt) can give you several hundred milligrams in one serving. The naturally aged, more artisan cheese also provide vitamin K2, which is important for directing calcium into bones rather than soft tissues and arteries. Among the non-dairy foods, the highest content will be from animal foods than have bony residues: bone-in fish (canned salmon and sardines for ex), bone-in slow cooked meats, and traditional both broth. I grew up with traditional foods and we never wasted any bones. A lot of folks make their own bone broth, but if you do not like your house smelling like soup all the time, you can purchase high quality broth in many natural food stores (Kettle and Fire brand for ex). Leafy green veggies and the brassica family (cabbage, broccoli,) also have a decent content, but the bio-availability is low so you need to eat them lightly cooked and preferably with a little fat. Otherwise, there are lots of foods that have a small amount of calcium that add up, so a varied whole foods diet will give you a few extra hundred mg per day.
PHOSPHORUS: Needs a special mention. Not because it is often deficient in folks diet. Phosphorus is a common additive in processed foods and sodas and not labeled as such. Phosphorus in processed foods is in such concentration that it upsets the balance of calcium and phosphorus in the intestines, causing salt precipitation of the two minerals together and preventing them from being absorbed. Bottom line, any processed food will negatively affect your calcium balance.
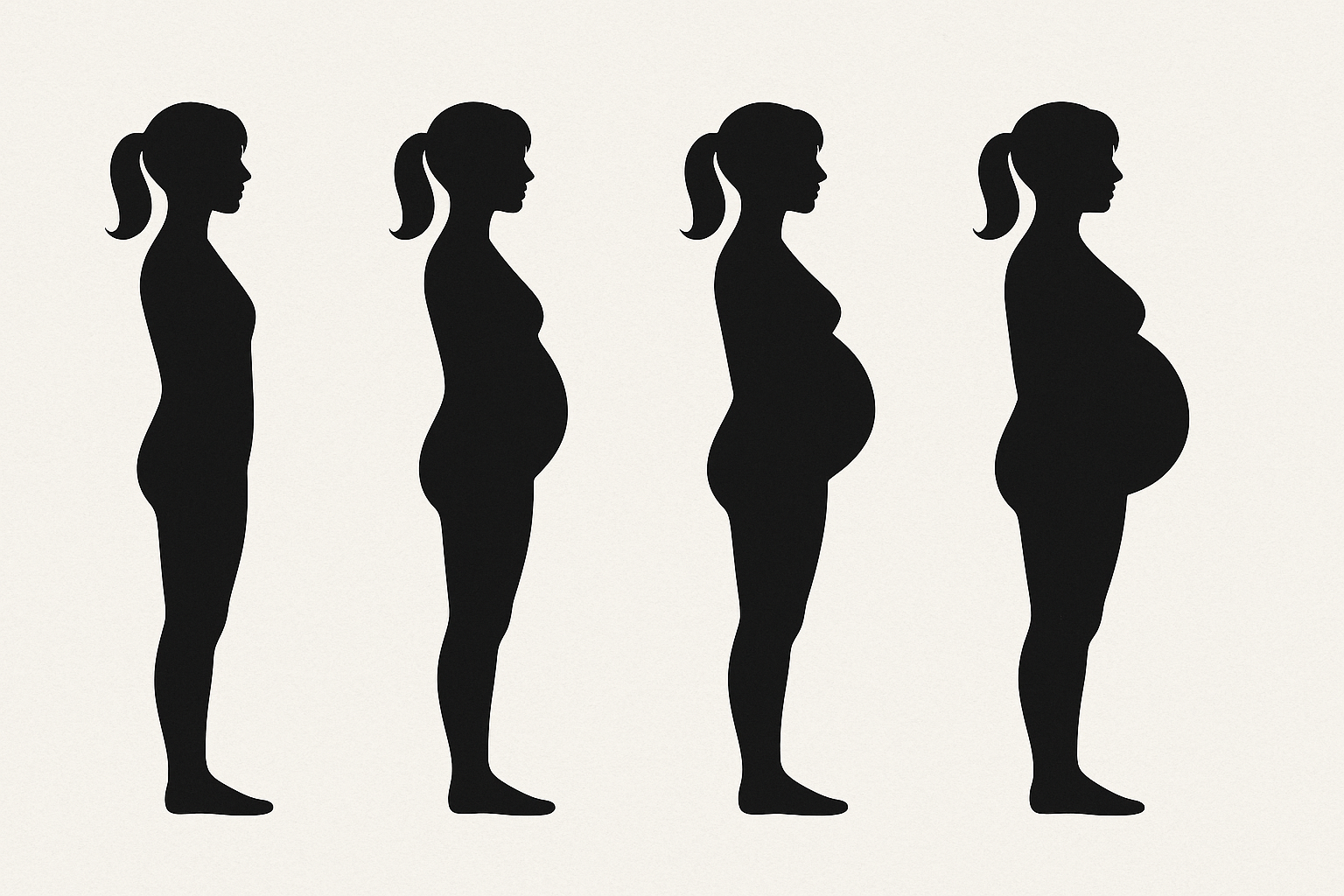
PROTEIN: Most of the scaffold of your bone is made out of collagen protein. Most of us need about 2/3 of our body weight in grams (150 lbs = 100 gr). You may need more in circumstances like illness, pregnancy, and intense physical activity. Protein needs to come from both plant and animal foods. There is a misconception floating around that animal protein make you lose calcium in your urine. That is not correct. Your body excretes extra calcium it does not need in the urine and animal protein significantly increases the rate of calcium absorption in the intestines, thus leading to a little more spillover in the urine. Animal protein should ideally include some of the soft tissues like skin and tendon because of the collagen amino acids that is incorporated in bones.
FAT SOLUBLE VITAMINS: Your body needs ALL fat soluble vitamins, not just vitamin D3. Vitamin D3 is ideally produced in your skin when cholesterol rings are converted by exposure to UV light. So you need some good sources of cholesterol and some time outside showing a little skin. Vitamin A is often the forgotten fat soluble vitamin, you need both plant and animal sources for optimal status. Vitamin K2 is also not getting enough attention for its role in balancing calcium deposition away from soft tissues and into bones. Highest levels are found in cheese, and fermented products (including some that are not common in the non-ethnic US diet). Fat soluble vitamins tend to be low in patients on vegan diets and on meds that limit the rate of fat absorption like statins
MINERALS AND TRACE MINERALS: Magnesium, zinc, and boron are all important in bone metabolism. Whole foods diets will usually give you enough, but for some folks it may need to be supplemented, especially magnesium.