https://www.npr.org/sections/health-shots/2021/10/07/1044010141/diet-soda-may-prompt-food-cravings-especially-in-women-and-people-with-obesity
In the busyness of life, I don’t always have the time or energy to crusade on all of my favorite pet peeves. There was a time in the past when I was much more proactive in spreading the word on the health risks of artificial sweeteners, and it is time to get back on my high horse about it.
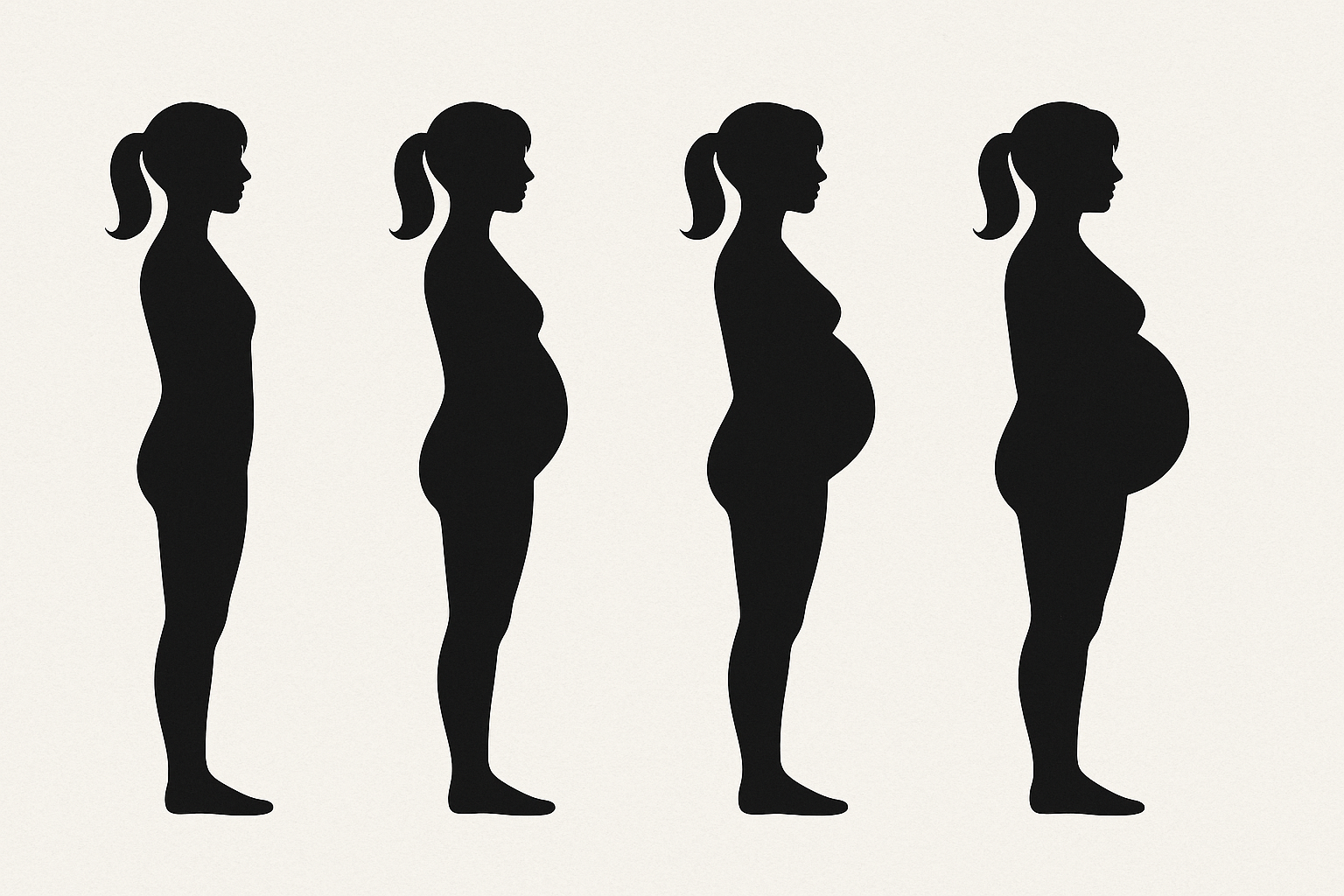
The stakes are not negligible. The processed food and diet industry has done a great job at making us believe those fake sugars are benign or part of a weight management strategy. They are neither. The article that was just featured in JAMA talks about the paradoxical increase in obesity among overweight and type 2 diabetic patients who consume sugar alcohol like sucralose focused on the metabolic and weight impact. while other studies have also shown how remarkably bad those artificial sweeteners are for your gut flora and all the functional digestive disorders that follow.
The recent research focused on the brain’s response to artificial sugar. Basically, it totally confuses your brain’s self regulating mechanisms of appetite, satiety, and blood sugar management: the brain assumes that sugar is coming to the blood stream when exposed to a sweet taste in the mouth, but when the two factors are delinked, the body stops properly producing leptin to signal that your are full or fails to produce the right amount of blood sugar regulating hormones at the right time and in the right amount.
Be on the lookout for the widespread presence of those artificial sweeteners in food, especially food that is labeled “light” This can be anything from yoghourt to dessert, salad dressing etc. The labels will clearly list it ( sucralose, Splenda). Also beware that a lot of packages listing stevia actually have added erythritol and sucralose as the first ingredient. Two safer alternatives in small amounts would be stevia and pure monk fruit powder. But in the end, you just have to limit your intake of sugar and there is no real way around it. Some supplements can help you achieve a lessened sugar craving, such as inositol or gymnema lozenges, and those do not contain artificial sweeteners